by Tom Malterre | 5 comments
If you don’t digest your food, your immune system may attack it.
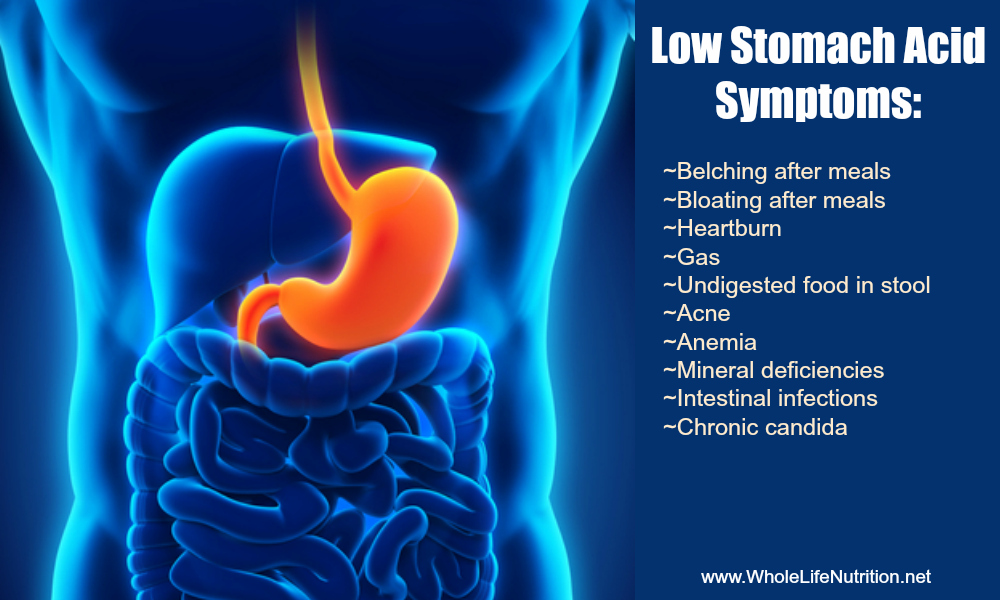
When we are healthy, we produce a strong acid in our stomachs; so strong that it resembles battery acid. This helps us to break apart our foods so we can access the nutrients found in them. But what happens when we have low acid in our stomach? We can’t break our foods down. This can lead to symptoms of indigestion, deficiencies of nutrients, and bacterial infections. Or, worst yet, your immune system attacks the food that hasn't been broken down leading to food allergies.
Digestive issues are so common; it’s likely that at least 25% of the people reading this article are suffering from GERD or dyspepsia (gas, burning, nausea, fullness, reflux, or general discomfort in your abdomen). Surprisingly, many of you that are taking medications for these issues may have caused food sensitivities and food allergies.
If you went to your doctor complaining of GERD or dyspepsia, you were most likely prescribed an acid blocking medication called a Proton Pump Inhibitor (PPI). From July 2013 to June 2014 there were 18.6 million monthly prescriptions written for the PPI Nexium® (the “Purple Pill”) in the US. In fact, it was the third most commonly prescribed medication in the country for that time period. Combined with another 4.6 million prescriptions of the PPI Dexilant® and countless over the counter purchases of Prevacid® and Prilosec®, chances are high that you or someone you know are taking one of these medications.
Research indicates a healthy person may start off with a pH in their stomach somewhere between 1.5 and 2.0. This is relatively equivalent to having battery acid in your stomach. Within 5 days of being on a PPI, this pH will shift to a 5 which is equivalent to table vinegar.
Unfortunately, the stomach was producing acid for a reason. All day the body is using a lot of energy (ATP) to guarantee that our acid level is 3 million times higher in our stomach than it is in our blood. This high acid content allows us to break apart bonds in the food we eat. This is one of the most important steps in the process called digestion. When we break apart our food properly in the stomach, the small intestines can then absorb the unlocked nutrients; bacteria and yeasts won't overgrow and cause dysbioisis, and the immune system won't have any large food particles to attack.
Science is showing that acid-blocking medications are increasing our risk for food allergies.
Numerous studies and FDA warnings are beginning to highlight that nutrient deficiencies of things like vitamin B12, iron, vitamin C, calcium, and magnesium often occur when people take acid blocking medications for long periods of time. But few people are talking about another side-effect of not breaking your food down: food reactions.
Food Allergies and Low Stomach Acid
It is estimated that over 70% of the body’s entire concentration of immune cells are found in the intestinal tract. These cells are designed to survey the contents of the intestines for possible foreign invaders like harmful bacteria or viruses. They often do this by recognizing certain amino acid sequences in the proteins of the substances that are traveling through. Just like we remember people by their facial features or personality traits, immune cells recognize organisms by their sequence of amino acids in their proteins. If there are amino acid combinations that look like harmful bacteria, fungi, viruses, or parasites, the immune cells will launch an “attack” against the foreign invader and call for reinforcements.
When proteins from our foods are properly digested, they are literally broken down into tiny fragments that contain 1, 2, or 3 amino acids. These substances are too small for the immune cells to mistake for a harmful organism and therefore they do not stimulate an immune response. If there is not adequate acid in the stomach, proteins are not broken down well. This leaves the protein fragments in a size and shape that can be mistaken for an invader and cause an immune reaction.
As Dr. Eva Untersmayr states in an article from Clinical Reviews in Allergy and Clinical Immunology, “Despite being considered a pleasure by most persons, food intake might also represent a health hazard in situations of altered metabolism or if food proteins are recognized as potentially harmful by the immune system.”
To test this theory, Dr. Untersmayer set up some experiments in petri dishes to see how important gastric acid's role was in lessening the allergenic capacity of foods. She found that proteins from cod fish lost their ability to bind to IgE antibodies within one minute of exposure to acids that were below a pH of 2.5. When the pH was raised slightly to a 2.75 (less acidic) that completely changed. In just that slight variation of acidity, the proteins became 10,000 times more likely to bind to IgE antibodies (meaning they became allergenic).
But does this theory hold up to scrutiny when we look at actual patients that take acid-blocking medications?
Dr. Untersmayr compared adults before and after a 3 month course of acid-blocking medication, she found that 10% of the subjects had an increase in existing IgE mediated allergies and 15% developed new allergies to foods like milk, potato, celery, carrots, apple, orange, wheat, and rye flour. “Thus, the relative risk to develop food-specific IgE after anti-acid therapy was 10.5.”
In other words, her subjects were 10.5 times more likely to develop food allergies when they are on acid blocking medications!
Babies and Children are More at Risk for Food Allergies
Is this the same for kids? Yes. A study in Pediatric Allergy and Immunology in 2013 examined what happened to children varying in age from 0-18 when they were on acid blocking medication for one year. When researchers compared 4724 children that were not on medications with another 4724 set of age-matched children that were on gastric blocking medications, they found a 367% increase in allergies in the medicated group.
If your baby has colic, the best option to reduce or eliminate symptoms is to have the breastfeeding mother do an Elimination Diet. If you are breastfeeding, there are many things you can do to get to the root of your infant's digestive issues. Removing the offending foods from your diet as well as adding in gut-healing nutrients can do wonders.
How to Heal after using Acid-Blocking Medications:
1. Amino Acids.
A healthy stomach will produce acid to break apart proteins so amino acids can be absorbed in the small intestines. When proteins are not broken down properly, amino acids are not absorbed properly. I find that many people are amino acid-deficient after being on these medications because of how they inhibit protein digestion. Slow cooked meats and bone broths are one option for increasing very digestible sources of amino acids, and so are amino acid supplements. The following amino acids have been shown to decrease muscle wasting and improve lean muscle mass for individuals that are deficient in protein:
Amino Acid Complex is a broad-spectrum amino acid supplement that was developed to decrease muscle wasting in cancer patients undergoing chemotherapy. It was later discovered to be effective at improving heart and mitochondrial function. There is actual research on this amino acid combination jump-starting mitochondrial function (you need to have good mitochondrial function so you can produce enough stomach acid). Purchase Amino Acid Complex in our online Store.
L-Glutamine is known to soothe the intestinal tract. In fact, it is the primary fuel for the intestinal cells! Glutamine also plays a roll in maintaining lean muscle mass. It is the most abundant amino acid in the human body and commonly used by athletes. Purchase L-Glutamine in our online Store.
2. Do an Elimination Diet.
Do you suffer from bowel flare-ups, skin problems, brain fog, insomnia, mood issues, muscle and joint pain, or migraines after being on your meds for 6 months or longer? Remember that acid-blocking medications cause low stomach acid, which then in turn allows for large, undigested food particles to reach the immune system. Food reactions cause a myriad of different symptoms.
If you are reacting to foods, it is going to be difficult to heal your body unless you remove those offending foods for a while. Our Elimination Diet has helped thousands of people identify what foods work and don’t work for their bodies. In the process, they have been able to let go of GERD, dyspepsia, joint pain, headaches, skin problems, mood issues, and more!
Have you read our book The Elimination Diet? As a companion to our book, we have an Elimination Diet Support Program that will guide you through the Diet. Click here to learn when our next group program begins (though you can join at any time).
3. Talk To Your Doctor.
Acid blocking medications may be necessary if you have a serious medical condition like stomach ulcers or Barret's esophagus. However, there have been numerous articles recently warning about the overuse of these medications for dyspepsia and GERD. They list numerous negative effects with the long-term use of acid blocking medications. Above and beyond food reactions, there have been warnings issued about an increase of bacterial infections (SIBO, c. difficile), magnesium deficiencies, fractures, community acquired pneumonia, vitamin B12 deficiencies, and more. If you have not discussed these with your doctor, now may be a good time to do so. Here are a few quotes and study links to help you communicate with your practitioner:
“…for most patients the adverse effects of PPIs outweigh the benefits. Reducing the unnecessary use of these medications will require action by both physicians and patients. As physicians, we should offer treatments other than PPIs for functional dyspepsia, prescribe short courses of PPI treatment (after disclosure of possible risks and benefits), and consider a trial of discontinuing PPI therapy in patients who are asymptomatic.” – JAMA Internal Medicine 2010 http://archinte.jamanetwork.com/article.aspx?articleid=415861
“Moreover, emerging data illustrate the potential risks associated with long-term PPI therapy including variations in bioavailability of common medications, vitamin B12 deficiency, Clostridium difficile-associated diarrhea, community-acquired pneumonia, and hip fracture. For these reasons, it is imperative to use the lowest dose of drug necessary to achieve desired therapeutic goals.” – Am J Gastroenterol 2009 http://www.ncbi.nlm.nih.gov/pubmed/19262544
"The authors concluded that PPIs are associated with a 29% increased risk of fracture, including 31% increased risk of hip fracture and a 54% increased risk of vertebral fracture. These findings were robust and were consistent across all types of studies, for both low- and high-quality studies, for both long-term use (defined as greater than 1 year) and any use, and for both usual doses and high doses." – Ann Fam Med. 2011 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3090435/pdf/0090257.pdf
4. Use The GERD Supplement Protocol.
Using this GERD supplement protocol is often more effective than using PPIs. In fact, it has helped hundreds of my clients heal from debilitating digestive issues. In this 2006 study, 176 GERD subjects were put on a supplement protocol and compared with 175 GERD subjects that were administered 20 mg of omeprazole (Prilosec®). At the end of 40 days, 100 percent of the patients in the supplement group reported relief of symptoms compared to 66 percent of the medication group. And here is where it gets fun. Once the initial 40-day trial ended, the researchers took the people who did not respond to the medication and gave them the supplements. All of 60 of them...100%...had resolution of their symptoms on the supplement protocol. Check out our GERD supplement package that contains these key nutrients for healing.
References
-
Brooks M. Top 100 Most Prescribed, Top-Selling Drugs. Medscape Medical News. Aug 01, 2014.
-
Prichard PJ, Yeomans ND, Mihaly GW, et al. Omeprazole: a study of its inhibition of gastric pH and oral pharmacokinetics after morning or evening dosage. Gastroenterology. 1985 Jan;88(1 Pt 1):64-9.
-
Untersmayr E, Jensen-Jarolim E. The role of protein digestibility and antacids on food allergy outcomes. J Allergy Clin Immunol. 2008 Jun;121(6):1301-8; quiz 1309-10.
-
Untersmayr E, Poulsen LK, Platzer MH, et al. The effects of gastric digestion on codfish allergenicity. J Allergy Clin Immunol. 2005 Feb;115(2):377-82.
-
Untersmayr E, Bakos N, Schöll I, et al. Anti-ulcer drugs promote IgE formation toward dietary antigens in adult patients. FASEB J. 2005 Apr;19(6):656-8.
-
Trikha A, Baillargeon JG, Kuo YF, et al. Development of food allergies in patients with gastroesophageal reflux disease treated with gastric acid suppressive medications. Pediatr Allergy Immunol. 2013 Sep;24(6):582-8.
-
Heidelbaugh JJ. Proton pump inhibitors and risk of vitamin and mineral deficiency: evidence and clinical implications. Ther Adv Drug Saf. 2013 Jun;4(3):125-33.
-
Katz, M. Failing the Acid Test; Benefits of Proton Pump Inhibitors May Not Justify the Risks for Many Users. Arch Intern Med. 2010;170(9):747-748.
-
Heidelbaugh JJ, Goldberg KL, Inadomi JM. Overutilization of proton pump inhibitors: a review of cost-effectiveness and risk [corrected]. Am J Gastroenterol. 2009 Mar;104 Suppl 2:S27-32.
-
Eom CS, Park SM, Myung SK, et al. Use of acid-suppressive drugs and risk of fracture: a meta-analysis of observational studies. Ann Fam Med. 2011 May-Jun;9(3):257-67.
-
Pereira RS. Regression of gastroesophageal reflux disease symptoms using dietary supplementation with melatonin, vitamins and aminoacids: comparison with omeprazole. J Pineal Res. 2006 Oct;41(3):195-200.

Stay up to date with the current science and recipes that can help make your family healthy.


Comments
H Pylori
by Sandra Robinson on Thu, 01/28/2016 - 12:56pm
Stomach Acid Ph Level
by Tamie on Fri, 05/19/2017 - 12:02pm
Hello,
by Moldovan Olesea on Thu, 01/10/2019 - 5:22am
root cause
by Judi on Wed, 09/25/2019 - 1:20pm
Food allergies
by Chloe on Sun, 03/22/2020 - 6:27pm
Add new comment